About the Pancreas
Source: This article was originally published by Mission:Cure here
What is the Pancreas?
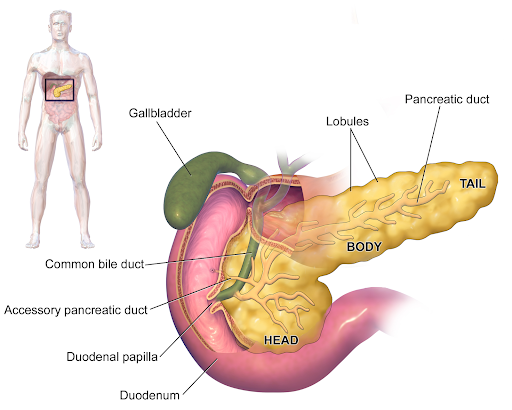
The pancreas is an organ that produces digestive enzymes to help digest food and insulin and glucagon to regulate blood sugar.
The pancreas is between 6 to 10 inches (15-24cm) long and sits in the upper left quarter of the abdomen, right behind the stomach.
This organ has important functions: it produces and releases the enzymes needed for digestion and regulates blood sugar levels.
What Does the Pancreas Do?
Producing Pancreatic Enzymes
The pancreas releases enzymes (pancreatic juice) into the small intestine. This is called the exocrine function. These enzymes help break down the food we eat. People who suffer from Exocrine Pancreatic Insufficiency (EPI) have impaired exocrine function, which means the pancreas does not secrete enough digestive enzymes.
Without enough pancreatic enzymes to break down nutrients, the body cannot properly absorb carbohydrates, proteins, and fats. This can lead to severe issues such as malnutrition, significant weight loss, and fat-soluble vitamin deficiencies. A low-fat diet and pancreatic enzyme replacement therapy or PERT (enzyme tablets consumed before and during each meal) can help patients suffering from this condition.
Regulated Blood Sugar Levels
In addition to producing digestive enzymes, the pancreas regulates blood sugar levels through its pancreatic islet cells. These cells generate and release insulin and glucagon.
If the body’s blood sugar level drops, the pancreas releases glucagon. This tells the liver to release stored glucose, which makes the blood sugar level rise again. If blood sugar levels are too high, the pancreas releases more insulin. Insulin is a hormone that helps absorb glucose, which causes blood sugar levels to drop.
Maintaining this balance is crucial – if insulin is no longer effective in bringing down blood sugar levels or if the pancreas does not release enough of it, it can lead to diabetes.
This visual is based on a graphic by Dr. Adrian Chabowski.
How Does Chronic Pancreatitis Damage the Pancreas?
Inflammation, diabetes and necrotizing pancreatitis
In people with chronic pancreatitis, the pancreas is constantly inflamed. The inflammation of the pancreas can cause scarring, which, in the long term, can destroy the pancreas that generate enzymes. This means that digestive enzymes can no longer be produced. This can lead to Exocrine Pancreatic Insufficiency (EPI).
As Guts UK Charity describes, the swelling and scarring of the pancreas can also cause an obstruction in the pancreatic ducts, the bile duct or the duodenum. To treat these obstructions, doctors will place stents (small drainage tubes) into the obstructed site.
Pancreatic inflammation can also damage the islet cells which produce insulin. As a result, the cells may not function well enough and the blood sugar level can remain too high. If that happens, diabetes can develop. It is called Type 3c diabetes.
In some cases, untreated acute pancreatitis can lead to necrotizing pancreatitis. This can also happen with untreated chronic pancreatitis, although less often. Necrotizing pancreatitis is caused when enzymes leak out of the inflamed pancreas and kill the pancreatic tissue. The symptoms of necrotizing pancreatitis include abdominal pain, nausea, vomiting and fever. If left untreated, the condition can become life threatening.
Can You Live Without a Pancreas?
Living without a pancreas is possible, but can be associated with other health concerns. There is no cure or treatment for chronic pancreatitis, and for some patients, the removal of the organ in a pancreas surgery is the only option. This is done in a surgery called Total Pancreatectomy and Islet-Autotransplantation (TPIAT). TPIAT usually involves the removal of the pancreas, the gallbladder, the spleen and part of the duodenum.
Without a pancreas, the body cannot produce insulin, making the patient immediately diabetic. To avoid or mitigate diabetes, the patient’s own insulin-producing islet cells are taken out of the pancreas and transplanted to the liver during the TPIAT surgery. However, success is not guaranteed, and some patients can remain dependent on insulin.
Is There a Treatment or Cure for Pancreatitis?
Enzyme replacement therapy and pain treatments are the only available treatments to relieve pancreatitis patients of their symptoms. Currently, there is no cure that stops or reverses pancreatitis, but Mission: Cure is working to find one so that all pancreatitis patients can live longer, happier, more productive lives – find out more here.